Personalized shot at stopping cancer
Clinical trials are using mRNA technology to develop personalized vaccines intended to prevent cancer from returning.

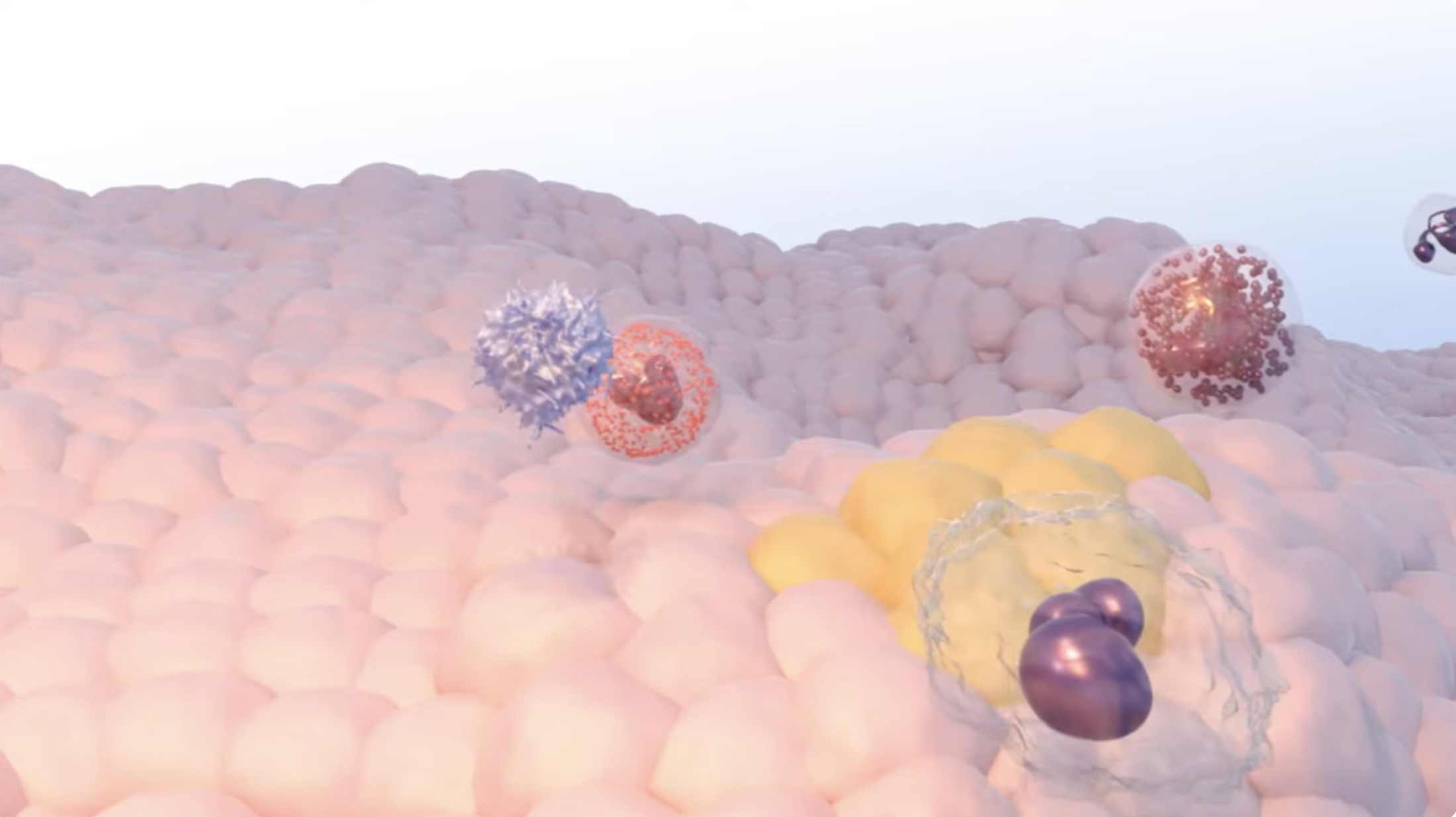
Immunotherapy is a simple yet powerful concept: Using the body’s own immune system to fight cancer.
The immune system is designed to protect you – to attack both foreign cells that could bring disease and any of your own cells that developed abnormally. Cancer cells are abnormal versions of your own cells, so the immune system should, and often does, attack them. But cancer cells also develop mechanisms to hide from the immune system – or even to trick the immune system into protecting the cancer. Immunotherapy aims to reverse this so the cancer can’t hide anymore.
There are many different kinds of immunotherapy. They use different methods, but all with the same goal: To get the immune system to target the cancer and to stay vigilant against any recurrences.
Some immunotherapies have completely changed how certain cancers are treated. And scientists are continuing to develop new immunotherapies and new types of immunotherapies to improve cancer treatment even more.
Hollings offers multiple clinical trials evaluating how to improve existing immunotherapies and extend their use to more types of cancer so that more patients can benefit from this new type of therapy.
Clinical trials are using mRNA technology to develop personalized vaccines intended to prevent cancer from returning.
A CAR-T cell therapy trial aims to make this therapy last longer with fewer side effects.
A Hollings patient is the first enrolled in a trial for a first-in-class bifunctional antibody.
National Cancer Institute video
The immune system has built-in safeguards – immune checkpoints – so that it doesn’t overreact. But some cancer cells use these checkpoints to shield themselves. Immune checkpoint inhibitors turn off, or inhibit, those checkpoints so that the immune system is unleashed.
Most people think of vaccines as something that you get so that you don’t become sick. There is a cancer vaccine like this. The human papillomavirus (HPV) vaccine protects against infection with this virus, which can cause six types of cancer.
There are also cancer vaccines that are given to people who have already had cancer to prevent the cancer from recurring. Just like regular vaccines use a distinctive feature of a virus to teach the immune system to recognize it, these cancer treatment vaccines use a distinctive feature of a cancer cell to train the immune system.
CAR-T cell therapy uses a patient’s own T cells and engineers them in the lab to add a CAR, or chimeric antigen receptor. T cells are part of the immune system. They’re already primed to attack invaders, but the CAR gives them a specific target on cancer cells to home in on. When the CAR-T cells are re-infused into the patient, they’re ready to target the cancer cells. So far, CAR-T cell therapy has been approved only for blood and lymphatic cancers.
National Cancer Institute video
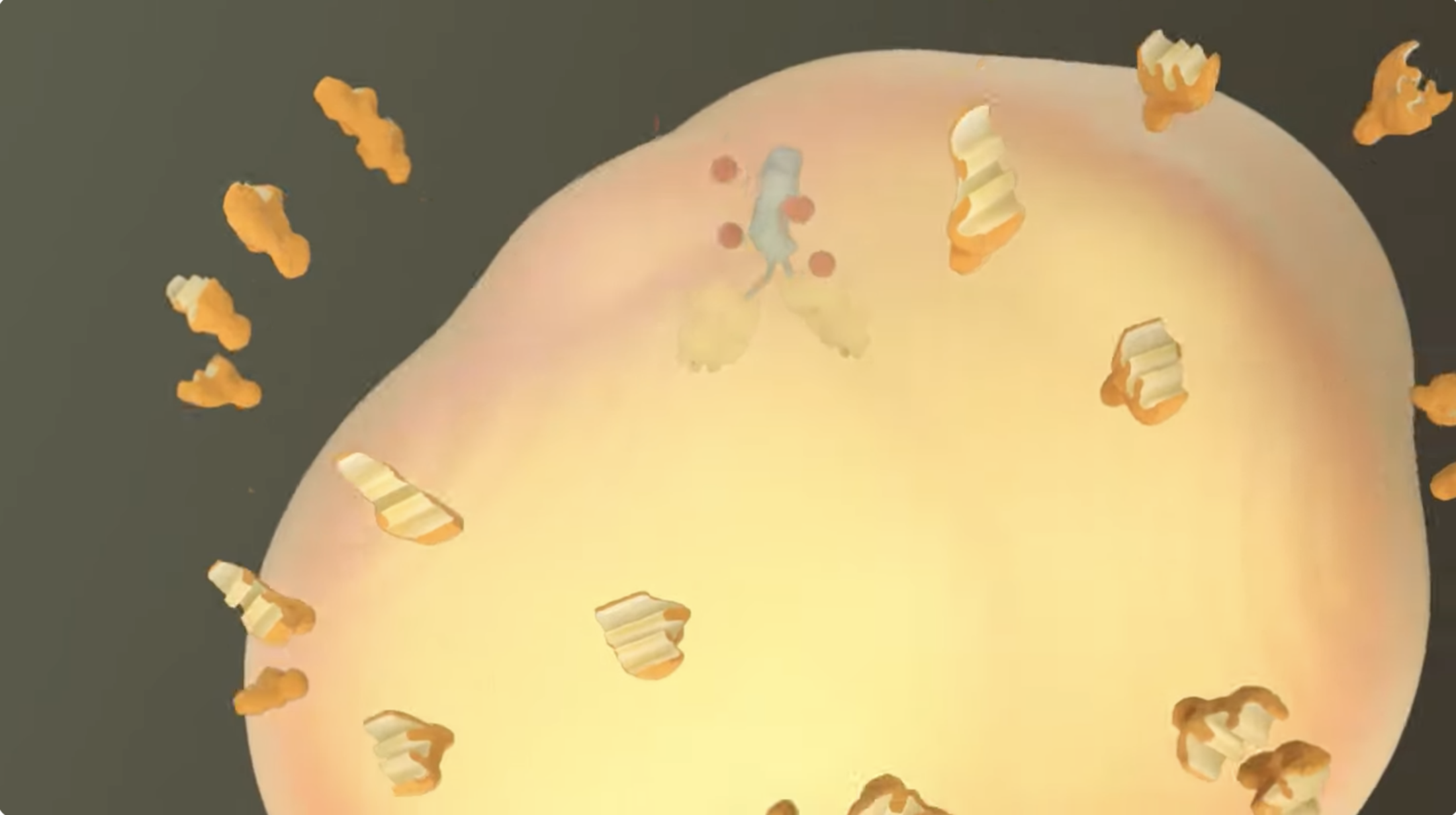
There are several ways that monoclonal antibodies are used in cancer treatment. Some of these methods are classified as immunotherapy, while other methods are classified as targeted therapy.
Monoclonal antibodies are antibodies that are made in the lab. They are all clones of a single starter antibody, which is why they are called monoclonal.
Some monoclonal antibodies act as markers. They attach to cancer cells, which helps to alert the immune system to their presence.
Other monoclonal antibodies have two arms – one arm attaches to the cancer and the other arm attaches to an immune cell, to physically bring the immune cell closer to the cancer cell.
Researchers are continuing to develop new types of monoclonal antibodies to target cancer.
There are lots of different chemotherapy drugs, just like there are lots of different immunotherapies. In general, though, chemotherapies are drugs that target cells that are growing and dividing quickly. This fits the description of most cancer cells, which are growing out of control. But it can also hit normal cells that divide quickly, which is why chemotherapy can cause people to lose their hair.
Most immunotherapies are given intravenously. That means the patient comes to an infusion center where a nurse inserts an IV and the patient sits while the immunotherapy is infused into the bloodstream.
Some immunotherapies, though, are given as shots. Immunotherapies that the patient takes by mouth are also being developed.
Often, these two types of drugs are given together. By working together, they have a better cancer-fighting effect.
Depending on the type of cancer, immunotherapy might be used before, during or after standard surgery and radiation treatments.
Immunotherapy is also part of the treatment plan for many cancers that are currently incurable.
One of the benefits of immunotherapy is that there are generally fewer side effects than chemotherapy – but there can be side effects.
Each treatment will have different side effects, depending on how it works inside the body. Some common side effects are fever, nausea, low blood pressure, rash, or fatigue.
CAR-T cell therapy can also cause more serious side effects like cytokine release syndrome or neurotoxicity.
Your doctor can explain the side effects that are expected with your specific treatment. If you are unsure, don’t hesitate to ask!
Immunotherapy can be used at all stages of cancer. But it’s important to remember that immunotherapies are developed for specific cancers at specific stages, so not every cancer will have a matching immunotherapy.