Our comprehensive approach and clinical expertise set us apart
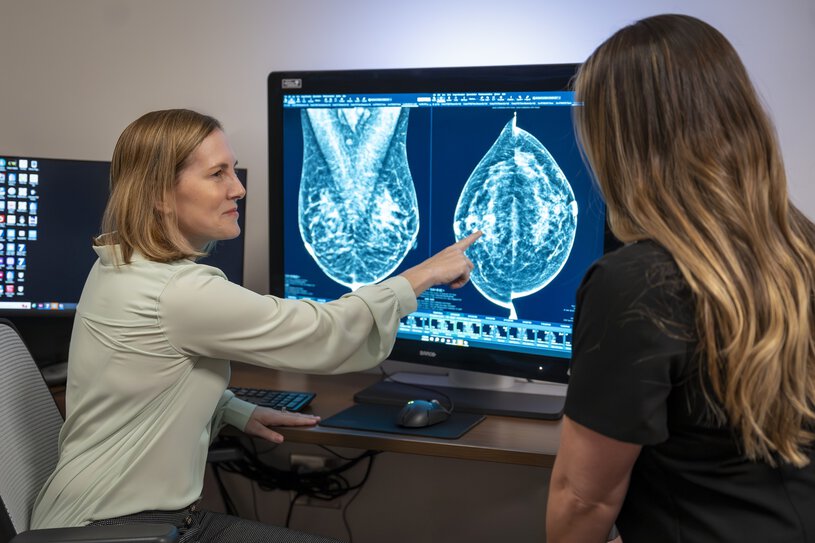
Breast cancer is the most common cancer diagnosed in women, after skin cancer. Likely you know someone who has had breast cancer — and perhaps now you’ve been told that you do, too. It can be scary to hear those words, but when detected early, breast cancer is a very survivable cancer, and the breast care specialists at MUSC Hollings Cancer Center are here for you.
Hollings fights back against breast cancer with the latest diagnostic technology, innovative treatment options, comprehensive care teams, and clinical trial opportunities. Our work doesn’t end with diagnosis. Our breast doctors aim to give you the best treatment and quality of life with compassion and support.