The most effective way to treat cervical cancer is to catch it early. When detected early and treated, cervical cancer is usually curable.
Women should begin getting screened for cervical cancer at the age of 21, regardless of when they become sexually active. There are a couple of different tests available. Here at MUSC Hollings Cancer Center, our general guidelines are for Pap tests every three years between the ages of 21 and 29. Beginning at age 30, assuming that no abnormal results have been found, we recommend co-testing every five years — that means getting both an HPV test and a Pap test. The HPV test is a newer test that detects HPV infection.
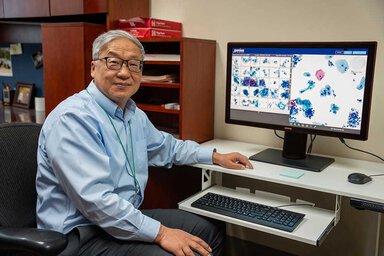
Collecting samples for these tests is the same process for both, and it happens during one procedure, so co-testing doesn’t mean an extra procedure for you. A doctor will insert a speculum into the vagina to widen it, then use a brush to collect cells from the cervix.
The above recommendations are general guidelines, but the frequency of screening can vary depending on your age and risk factors — talk to your doctor about the best options for you.
Cervical cancer screening
To get screened, talk with your primary care doctor or schedule a gynecology appointment online.
Pap test for cervical cancer
The Pap test, also called a Pap smear, has helped to reduce cervical cancer death rates by 86%. For a Pap smear, the cells collected during the test are viewed under a microscope to see if precancerous cells or cancer cells are present. Often, it takes years for precancerous cells to develop into caner. Finding these cells while they are still precancerous means you can have them removed before you ever get a cancer diagnosis.
HPV test for cervical cancer
The HPV test looks for DNA or RNA from high-risk types of HPV. There are more than 100 different strains of HPV. This test looks for the types most likely to cause cancer. Even if the test is positive, it doesn’t mean that you have cancer. It means that you are at higher risk of cancer, and your doctor may order additional tests or more frequent tests so that you can be treated if the infection begins to develop into cancer.